Virtual Patient Simulation (VPS) Case Study in AF
CME Using VPS Improves Diagnosis and Management of Atrial Fibrillation
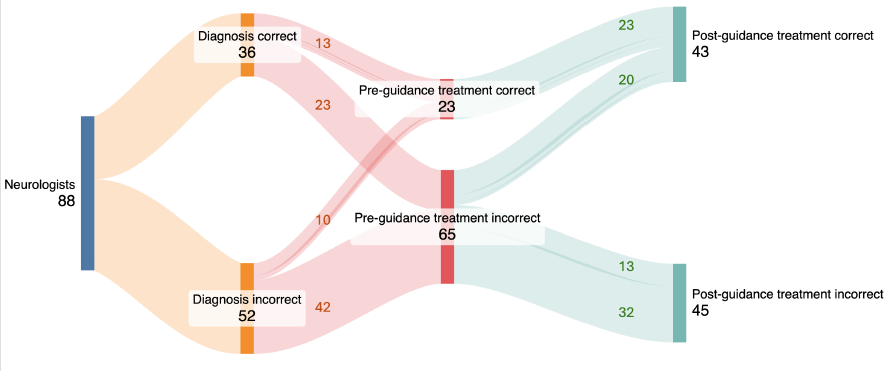
Our latest study shows the power of virtual patient simulation in closing critical gaps in medical education. We saw significant improvements in how cardiologists and PCPs diagnose and manage Atrial Fibrillation (AF). Below is a chart showing data from one patient case from the simulation.
Challenge
Diagnosis and management of atrial fibrillation (AF) often fall short of clinical best practice across both specialist and primary care settings. Prior to intervention, significant gaps existed in the timely and accurate diagnosis of AF, selection of anti-arrhythmic drug (AAD) therapy, and appropriate patient monitoring. Baseline data showed that up to 70% of cardiologists and 83% of primary care physicians (PCPs) made incorrect diagnostic choices, and the majority did not select the most appropriate AAD in patients with AF based on the latest clinical evidence and guideline-based strategies.
Solution
A case-based, virtual patient simulation (VPS) intervention was deployed, enabling 1,599 participating cardiologists and PCPs to make diagnostic, testing, and treatment decisions for two complex AF cases. The VPS system included real-time clinical guidance (CG) based on expert, evidence-based recommendations and allowed physicians to revise their decisions post-feedback. Learners’ pre- and post-intervention choices were rigorously analyzed using McNemar’s test.
Impact
Diagnostic Accuracy: Timely and correct diagnosis of AF improved significantly for both cardiologists (from 30% to 66%) and PCPs (from 17% to 48%), with overall improvement from 16% to 57% (P < .001) for one case scenario with similar improvements in the second patient case as well. (P < .001)
Therapeutic Selection: Selection of appropriate AAD therapy rose among all specialties after guidance (P<.001), but a notable gap persisted across both patient cases where up to 40% of cardiologists and PCPs still did not select an AAD for the clinical scenarios despite improved performance, respectively.
Monitoring Strategies: Use of correct monitoring improved for cardiologists (from 40% to 62%; P<.001) and PCPs (from 32% to 55%; P<.001).
Sustained Gaps: VPS with immediate clinical guidance improved learners’ clinical decision-making related to the evidence-based diagnosis and management of AF with AADs. It also pinpointed that a gaps remained with a substantial proportion not making optimal decisions post-intervention, signaling areas for ongoing educational investment.


Conclusion
VPS-based CME demonstrably enhances AF diagnosis, treatment, and monitoring by physicians, but continued education is needed to fully close practice gaps, especially in rhythm control management.

 By
By