Where Are We Today With Artificial Intelligence (AI) in Rare Disease Diagnosis and Care?
Discover how AI-powered tools are transforming rare disease diagnosis, patient care, and clinical decision-making.
August 2025

Christy: Gareth, you’re active in so many projects in rare disease, but I want to focus on AI here. I’ve been fascinated with facial recognition tools that can be used to identify the unique facial features that are known to be associated with some 40% of rare diseases. What are your thoughts?
Gareth: Thanks, Christy. Well, one thing to consider is that all the tools at the moment are really set up as diagnostic support tools. So, they're set up to be used together with the clinician's knowledge and in combination with say, a genetic diagnostic to get confirmation, not as a standalone thing. That said, some of the examples, particularly for facial recognition, include GestaltMatcher, Face2Gene, and Cliniface.
Christy: And what other AI-based approaches can help shorten the rare disease diagnostic odyssey?
Gareth: There's no doubt that generative AI approaches have really moved the needle, and there's now almost a flood of generative AI approaches for helping to analyze genomic and other data, so I think that that's really promising.
However, still the most useful tools we have are what we were taught in medical school: take a good history, do a good examination, listen to the person and family in front of you, and ensure continuity of care. This basic approach has become even more important today because there are amazing AI-based technologies, but the scale at which they can generate right answers and the scale at which they can generate wrong answers have both gone up.
Christy: What are the main challenges in using AI in rare disease?
Gareth: The reality is that people use lots of AI tools now to try and make diagnosis. People will be on ChatGPT or other platforms, sticking in their symptoms just like they did with Google before. But there are “hallucinations” that generative AI makes up that can sound incredibly plausible. If you’re an expert, you might have the experience to say, “Well that’s just wrong,” or “that doesn’t sound right to me.” So, it's thinking about how to use these things responsibly. There are so many people without a diagnosis. It's trying to serve that unmet need, but we also need to do it in a way that maximizes benefit and minimizes harm.
Christy: What AI applications do you find most exciting for rare diseases?
Gareth: Where I think there are potentially more scalable solutions that will help across the whole rare disease experience is using AI to better plan care across the lifespan. Through the International Rare Disease Research Consortium (IRDiRC), we wrote a framework on this. We’ve shifted a lot of our focus to using AI to create personalized care plans for people across the entire lived experience including health, education, and disability service provision. We call this a cross-sector approach to care. This is really important because there are 10,000 different rare disorders, so how would you expect a clinician to suddenly be able to generate a care plan on a particular condition for a child of a specific age with X,Y, Z features? And that’s what we’re increasingly able to tackle with UTOPIA. UTOPIA is an acronym for Unlocking Treatment Options Personalized In-Time Access.
Christy: Tell me more about UTOPIA.
Gareth: Well, it’s about putting accurate information into the hands of clinicians in a faster way. Instead of having to take hours searching, we can generate that information from trustworthy sources using AI. That is then available for the clinician ahead of seeing the patient and family so they can work in a more informed, efficient, and personalized way together with the patient and family and then present that information in a way that is easier to understand and use. And a core principle of UTOPIA is to ensure that solutions are equitable and globally accessible, adapting to diverse environments and peoples. It is certainly not perfect, and we strive to continually improve the approach. We are always on the outlook for people with the time and talent to help.
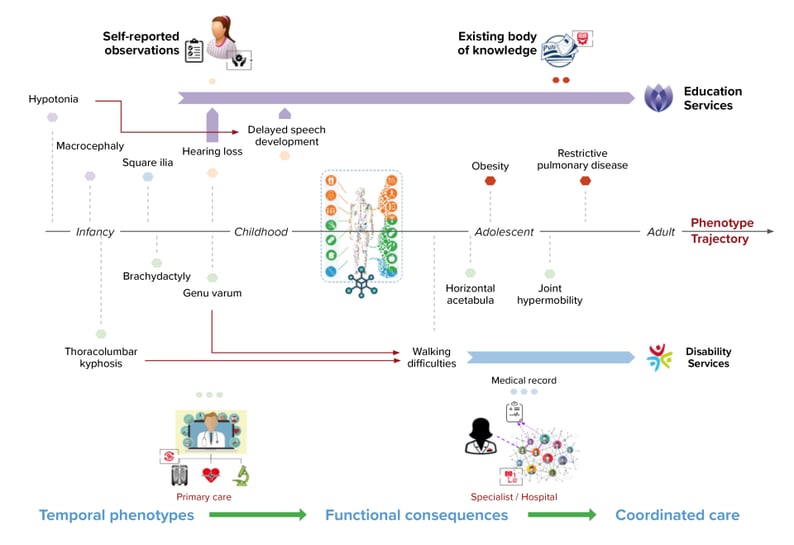
The below diagram shows how features of a particular disease typically evolve over time [middle of the diagram]. UTOPIA puts information together by combining the power of the patient and family voice, the expertise of the clinicians, trustworthy sources of knowledge like medical publications and various other information sources, and AI. UTOPIA uses this to create computational natural histories of disease. It connects knowledge on a condition and an individual’s disease features at different points in time and how features evolve over time (temporal phenotypes). And this is linked through to their (functional) consequences, meaning how individuals are affected or are likely to be affected in terms of function. This combination is then used to plan care across multiple sectors including health, disability, education—so a cross-sector approach for coordinated care.
Christy: That sounds like it can really make a difference for rare disease patients and families. Thank you so much for the conversation, Gareth!
References- https://www.sciencedirect.com/science/article/abs/pii/S0002929725001351
- https://globalrarediseasecommission.com/utopia-innovative-digital-ai-platform-improves-care-for-children-with-diagnosed-and-undiagnosed-rare-diseases/
- https://www.sciencedirect.com/science/article/pii/S2950008724000401

 By
By